On This Page:
Background
Medicaid enrollees have a higher smoking prevalence than the general population. Smoking-related diseases are a major contributor to Medicaid costs. Providing people who use tobacco with access to evidence-based tobacco cessation treatments can reduce morbidity and mortality from cancers and other tobacco-related diseases and reduce Medicaid costs. Individual, group, and telephone counseling are effective in helping people who use tobacco to quit. In addition, the U.S. Food and Drug Administration (FDA) has approved seven medications for smoking cessation, including five nicotine replacement therapies (the nicotine patch, gum, lozenge, nasal spray, and oral inhaler*) and two non-nicotine medications (bupropion and varenicline). The U.S. Surgeon General has concluded that, with adequate promotion, comprehensive, barrier-free, insurance coverage of evidence-based cessation treatment increases both the availability and use of cessation services, leads to higher rates of successful quitting, and is cost-effective.
There is considerable variation in states’ Medicaid insurance coverage of tobacco cessation treatments for standard (vs. expansion) Medicaid enrollees. All state Medicaid programs are required to cover tobacco cessation services (both counseling and medications) for pregnant women under section 4107 of the 2010 Patient Protection and Affordable Care Act (ACA). Additionally, effective 2014, section 2502 of the ACA barred state Medicaid programs that participate in the Medicaid drug rebate program from excluding coverage for cessation medications approved by the FDA. Telephone counseling is available for free to callers to state quitlines (including Medicaid enrollees) in all 50 states and the District of Columbia via 1-800-QUIT-NOW. However, coverage of individual and group cessation counseling for non-pregnant standard Medicaid enrollees varies widely by state. As of December 31, 2024, only 26 states provided comprehensive insurance coverage of all evidence-based cessation treatments (all seven FDA-approved smoking cessation medications, individual and group cessation counseling) for standard Medicaid enrollees. Expansion of treatment coverage while reducing barriers to treatment access (e.g., copays, duration limits on treatment) is still needed.
Measure
The number of state Medicaid programs that provide comprehensive insurance coverage of evidence-based tobacco cessation treatments (all seven FDA-approved smoking cessation medications plus individual and group cessation counseling) for standard Medicaid enrollees.
The number of state Medicaid programs that provide insurance coverage for individual or group tobacco cessation counseling for standard Medicaid enrollees.1
The number of state Medicaid programs that provide insurance coverage for all seven FDA-approved smoking cessation medications including the nicotine patch, nicotine gum, nicotine lozenge, nicotine nasal spray, nicotine oral inhaler*, bupropion (Zyban®) and varenicline (Chantix®) for standard Medicaid enrollees.1
*Manufacturing of the oral inhaler was discontinued in September 2023.
1Definitions
Standard Medicaid Enrollees: Persons who are enrolled in Medicaid under standard Medicaid eligibility criteria; does not include enrollees who are eligible under the income-only eligibility criteria for expanded Medicaid coverage.
Covered (individual counseling, group counseling): Service was covered for all standard Medicaid enrollees, including those enrolled in fee-for-service and managed care plans.
Varies (individual counseling, group counseling): Service coverage was different between managed care and fee-for-service plans, coverage varied among fee-for-service plans or among managed care plans, or coverage varied by pregnancy status.
Not Covered (individual counseling, group counseling): This service was not covered under applicable fee-for-service and managed care plans, or information was not available for both plans.
Covered (smoking cessation medications): All seven FDA-approved smoking cessation medications were covered for all standard Medicaid enrollees, including those enrolled in fee-for-service and managed care plans.
Varies (smoking cessation medications): Coverage of all seven FDA-approved smoking cessation medications was different between managed care and fee-for-service plans, coverage varied among fee-for-service plans or among managed care plans, or coverage varied by pregnancy status.
Not Covered (smoking cessation medications): Any of the seven FDA-approved smoking cessation medications was not covered under applicable fee-for-service and managed care plans, or information was not available for both plans.
Data Source
Centers for Disease Control and Prevention. State Tobacco Activities Tracking and Evaluation (STATE) System. Annual quarter 4 estimates through 2023.
Unpublished data for Q4, 2024 provided by the American Lung Association.
Healthy People 2030 Target
- Increase comprehensive Medicaid insurance coverage of evidence-based treatment for nicotine dependency to include all 50 U.S. states and the District of Columbia.
Healthy People 2030 is a set of goals set forth by the Department of Health and Human Services.
Trends and Most Recent Estimates
- Comprehensive Coverage of Cessation Treatments
-
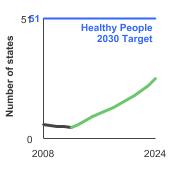
Number of states (including the District of Columbia) with comprehensive Medicaid insurance coverage for evidence-based tobacco cessation treatments, 2008-2024 Overview Graph Detailed Trend Graphs Most Recent Estimates (2024) Number of states 95% Confidence Interval 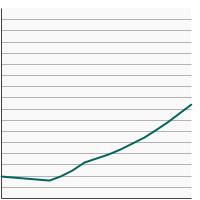

Comprehensive Coverage of Cessation Treatments 
26.0 Not available - Group Cessation Counseling
-
Number of states (including the District of Columbia) with Medicaid insurance coverage for group tobacco cessation counseling, 2008-2024 Overview Graph Detailed Trend Graphs Most Recent Estimates (2024) Number of U.S. states 95% Confidence Interval 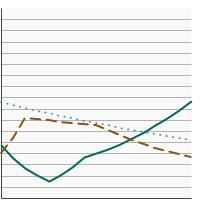

Covered 
26.0 Not available Varies 
11.0 Not available Not Covered 
14.0 Not available - Individual Cessation Counseling
-
Number of states (including the District of Columbia) with Medicaid insurance coverage for individual tobacco cessation counseling, 2008-2024 Overview Graph Detailed Trend Graphs Most Recent Estimates (2024) Number of U.S. states 95% Confidence Interval 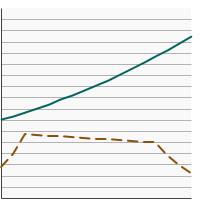

Covered 
44.0 Not available Varies 
7.0 Not available Not Covered 
0.0 Not available - Smoking Cessation Medications
-
Number of states (including the District of Columbia) with Medicaid insurance coverage for all seven FDA-approved smoking cessation medications, 2008-2024 Overview Graph Detailed Trend Graphs Most Recent Estimates (2024) Number of U.S. states 95% Confidence Interval 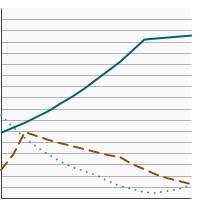

Covered 
43.0 Not available Varies 
4.0 Not available Not Covered 
4.0 Not available
Additional Information
- Tobacco and Cancer. American Cancer Society.
- Surgeon General’s Reports on Smoking and Tobacco Use. Centers for Disease Control and Prevention.
- Tobacco Cessation. Medicaid.gov.
- Tobacco Products. U.S. Food and Drug Administration.
Quitting Resources
- Tobacco. National Cancer Institute.
- Smokefree.gov. National Cancer Institute.
- How to Quit Smoking or Smokeless Tobacco. American Cancer Society.
- How to Quit Smoking. Centers for Disease Control and Prevention.
- Treating Tobacco Use and Dependence: 2008 Update. Agency for Healthcare Research and Quality.
- Healthcare Provider Resources: Smoking and Tobacco Use. Centers for Disease Control and Prevention.
- Tobacco Use. Million Hearts.
- North American Quitline Consortium.
- State Medicaid Coverage for Tobacco Cessation Treatments and Barriers to Accessing Treatments – United States, 2018-2022. DiGiulio A, Tynan MA, Schecter A, Williams KS, VanFrank B. MMWR Morb Mortal Wkly Rep 2024;73:301–306.
- Policies affecting Medicaid beneficiaries’ smoking cessation behaviors. Brantley E, Greene J, Bruen B, Steinmetz E, Ku L. Nicotine Tob Res 2018:00(00):1-8.
- The Affordable Care Act Medicaid Expansion and Smoking Cessation Among Low-Income Smokers. Donahoe JT, Norton EC, Elliott MR et al. Am J Prev Med 2019;57(6):e203-e210.
- Impact of Medicaid expansion on smoking prevalence and quit attempts among those newly eligible, 2011-2019. Hilts KE, Blackburn J, Gibson PJ, et al. Tob Prev Cessat. 2021 Aug 5;7:16.
- Does state Medicaid coverage of smoking cessation treatments affect quitting? Kostova D, Xu X, Babb S, McMenamin SB, King BA. Health Serv Res 2018;53(6):4725-4746.
- How Medicaid and other public policies affect use of tobacco cessation therapy, United States, 2010–2014. Ku L, Brantley E, Bysshe T, Steinmetz E, Bruen BK. Prev Chronic Dis 2016;13:E150.
- Helping smokers quit—opportunities created by the Affordable Care Act. McAfee T, Babb S, McNabb S, Fiore MC. N Engl J Med 2015;372:5–7.
- The Affordable Care Act's Medicaid Expansion and Impact Along the Cancer-Care Continuum: A Systematic Review. Moss HA, Wu J, Kaplan SJ, Zafar SY. J Natl Cancer Inst. 2020 Aug 1;112(8):779-791.
- Current smoking and quit-attempts among US adults following Medicaid expansion. Valvi N, Vin-Raviv N, Akinyemiju T. Prev Med Rep. 2019; epub.
- Smoking prevalence in Medicaid has been declining at a negligible rate. Zhu SH, Anderson CM, Zhuang YL et al. PLoS One 2017;12(5): e0178279.
- Current Use of Cigarettes in the United States: The Joint Role of Race/Ethnicity and Health Insurance Coverage. Soulakova JN, Crockett LJ. Healthcare (Basel). 2023 Nov 21;11(23):3014.
- Current Cigarette Smoking Among Adults in the United States. Centers for Disease Control and Prevention.
- State Tobacco Activities Tracking and Evaluation (STATE) System: Map of Comprehensive Medicaid Coverage of Cessation Treatments. Centers for Disease Control and Prevention.